Quick overview :
Spinal canal stenosis or spinal canal narrowing
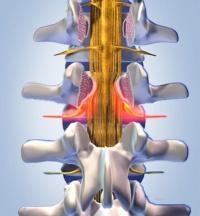
In the case of spinal canal stenosis, also known as spinal canal narrowing, various anatomical structures are often involved, which together form the wall of the spinal canal: due to degenerative changes in vertebral joints, ligaments and intervertebral discs, the spinal canal narrows and often also the bony nerve exit openings (foramen). A direct narrowing occurs when a damaged intervertebral disc bulges backwards or protrudes.
In the case of pronounced signs of wear and tear on the vertebral joints, bony protrusions (spondylophytes) form, which then narrow both the spinal canal and the nerve exit openings. Another cause is an abnormal thickening of the ligaments between the vertebrae that stabilize the spine (ligamentum flavum). All degenerative changes result in the space for the nerves running in the spinal canal becoming increasingly narrow over time until they are literally squeezed.
What causes spinal canal stenosis?
To a certain extent, spinal canal stenosis / narrowing of the spinal canal is a typical aging phenomenon of the spine; Many years of incorrect or excessive strain, such as the frequent carrying of heavy objects and other back-straining activities promote the development of spinal canal narrowing. Typically, the symptoms appear in active patients around the age of 50.
If there is no therapeutic intervention, there is a risk of nerve failure!
Common symptoms associated with spinal canal stenosis
- Back pain radiating down the leg
- Severe discomfort when walking longer distances
Sometimes no more 100 meters possible without a longer break - Numbness in the buttocks and/or legs
- Aggravation of pain in stretched posture
- Your pain is relieved by bending over or sitting down
Careful diagnosis of spinal canal stenosis is a prerequisite for successful treatment
Which procedure makes sense in individual cases depends on the diagnosis. Although the description of the symptoms usually points the way, clarity is often only brought about by imaging procedures such as computer or magnetic resonance imaging. It is important to know the degree of spinal damage and to know how many segments are affected by the narrowing. It is also important to determine whether there is already instability in the spine, whether and to what extent bony outgrowths must be surgically removed, or whether the desired relief can be achieved, for example, with the use of an implant.
In principle, any section of the spine can be affected by a narrowing; by far the most commonly affected area is the lumbar spine.
How is spinal stenosis treated?
Conservative treatment
In the case of minor complaints, it can be helpful to consistently rest your back and treat the pain with medication. A physiotherapeutic program under professional guidance is recommended to strengthen the back and abdominal muscles; accompanying heat treatments, electrotherapy and manual therapy can provide relief. Sometimes injections of local anesthetics and cortisone preparations next to the constricted nerve root (periradicular infiltration) can also be indicated. Special girdles and corsets are available from specialist retailers that bring the affected section of the spine into a more favorable curvature and thus also help to reduce the symptoms.
Surgical treatment without STIFFENING
If the complaints and neurological symptoms cannot be controlled with conservative measures, surgical treatment is necessary, through which the spinal canal is surgically expanded through targeted relief measures, such as the removal of constricting structures, so that the affected nerves are free again.
Microscopic decompression
Endoscopic decompression in stenosis
If there is only a narrowing of the nerve exit hole (foramen stenosis), there is the possibility of endoscopic decompression (expansion) with the additional use of a laser. Here, under endoscopic control and visibility, the structures constricting the nerve hole are removed in a particularly gentle manner, thereby relieving the pressure on the nerve.
This procedure should only be performed by a highly experienced and skilled spinal surgeon.
This is a minimally invasive procedure that can be performed under local anesthesia!
!!! The success is largely dependent on the experience of the operator !!!
Endoscopic decompression
Operative expansion through spacers
In very rare cases, it may be sufficient to widen the narrowed spinal canal (spinal canal stenosis) using special implants that are inserted between the spinous processes of two adjacent vertebral bodies. These spacers (spreaders) literally push the spinous processes apart and thus ensure the desired relief of the narrowed spinal canal.
The procedure takes about 30 minutes and is generally performed under general anesthesia. Immediately afterwards, the patients usually feel a significant reduction in symptoms. The day after the operation, the patient can get up; wearing a lumbar support girdle for four weeks protects against incorrect movements. Working at a desk is possible after two to three weeks, physically demanding activities are possible again after six weeks.